By A Midwestern Doctor
The Forgotten Side of Medicine
April 28, 2025
Many of the problems we currently see in medicine are not new, but rather iterations of things that have been forgotten and occurred countless times in the past. For example, the COVID mRNA vaccines are not the first time the medical field has experienced irrational exuberance for a dubious remedy, even as some of their colleagues spoke out against it (at great risk to their professional standing). Here, we'll look at what happened with corticosteroids, both because it provides a critical window into much of what's gone awry with medicine and because steroids are some of the most problematic but widely used medications on the market.
Allopathy
Because of the work that has been done to enshrine our system of medicine as the gold standard everything else must measure up to, many are not aware it is just one of many approaches to healing that has been developed throughout history, or even that in previous eras, it had its own label rather than just being "medicine."
Note: one of the major challenges I run into when writing is that there is no widely accepted term for our system of medicine, as they either simply assert it is "the standard" (e.g., conventional medicine or modern medicine) or frame it in a cultural context (e.g., "Western Medicine"). Of the accepted options, "biomedicine" is probably the most accurate (but largely unknown to the general public), whereas "standard medicine" (a term I made up) has become my favorite as it encapsulates it being the orthodox approach, the need of medicine to treat patients through standardized algorithms that ignore their individuality, and highlights J.D. Rockefeller's monopolization of medicine in the early 1900s (as he named his oil monopoly "Standard Oil").
Almost two thousand years ago, Galen, a Greek physician in Rome, collated, systematized, and refined existing approaches to medicine, particularly those originating in Greece, and then disseminated them worldwide. Central to Galen's approach were the importance of anatomy (gained through continuous dissections) and the humoral theory of disease, which dominated Western medicine until around the 1850s.
For context, Hippocrates' humoral theory of disease posited that health depended on the balance of four bodily fluids, known as humors: blood, phlegm, yellow bile, and black bile. Each humor was associated with specific qualities (hot, cold, wet, dry), elements (air, water, fire, earth), and temperaments (sanguine, phlegmatic, choleric, melancholic). Within this framework, disease resulted from an imbalance of these humors, caused by factors such as diet, environment, or lifestyle. Treatments, including bloodletting, purging, and dietary changes, aimed to restore humoral balance.
While this framework somewhat resembled what other cultures had come up with (e.g., the "fire" of the five elements in Chinese Medicine and "Pitta" of Ayurveda largely matched "yellow bile"), like surgery, it was more unique in its tendency to use forceful measures to correct a perceived humoral imbalance in the body. This in turn, gave way to a system of medicine where drugs that created dramatic physiologic changes (e.g., mercury, lead, arsenic, and opium) became the therapeutic mainstays of Western medicine, particularly since it was much easier to tell a drug "worked" if it created a dramatic effect.
Unfortunately, in many cases, those dramatic effects (e.g., it rapidly inducing vomiting) were due to the drug being highly toxic so many were injured by these early drugs, which in turn required the medical profession to aggressively double-down on the importance of their approach (particularly since so many people were being severely poisoned by mercury based drugs).
Note: during my training, another doctor proudly showed me the bag his father had brought to many visits, and sure enough, it had mercury in it (which remarkably the doctor did not even realize was mercury).
Because of the poor outcomes this form of medicine often produced, a variety of alternative approaches came into existence (e.g., Homeopathy in 1796, Eclectic Medicine in 1827, Osteopathy in 1874, Chiropractic in 1895 and Naturopathy in 1901), all of which were based on supporting the body's ability to heal itself rather than trying to force the body into its desired state. To cement this distinction, the founder of Homeopathy used the term "Allopathy," ("allo" means 'other' or 'different') as it highlighted allopathic medicine's tendency to use external interventions (e.g., drugs or surgery) that created effects opposite to the existing disease in order to bring the body towards its desire state.
Note: initially, Allopathy was a derisive term, but in time some MDs adopted it to distinguish themselves from their competition, however once Allopathy used a variety of monopolistic tactics around 1910 to take over the medical marketplace (which was necessary to save the dying profession), Allopathy faded into obscurity and Allopaths simply referred to themselves as "doctors" while Allopathic medicine became "medicine" (and all the other approaches to healing largely faded into obscurity despite many offering immense benefit to patients).
As Allopathic medicine evolved (e.g., new drugs were discovered) it gravitated towards drugs which suppressed the unpleasant symptoms in the body (e.g., fevers or skin eruptions), in part because this matched its pre-existing mentality of forcefully overriding illness and in part because this was the easiest way to create a dramatic change in a patient (hence inspiring confidence in both the doctor and patient).
At the same time however, the competing schools of medicine became more and more aware of the damage Allopathic remedies created and gradually concluded that while suppressing symptoms could lead to short term improvements, it often also lead to the subsequent creation of severe illnesses (which coincides with Allopathic medicine being excellent at treating acute emergencies but poorly equipped to treat chronic diseases).
A key insight during this debate ( Hering's Law of Cure) came from a Homeopath who concluded that healing occurs in a specific order (e.g., from the inside out, from the head down, and in the reverse order of symptom appearance) and that disease occurs in the opposite direction (e.g., initially at a superficial level and then eventually at a deep one). Thus, by allopathically suppressing symptoms (which were often the body's attempt to expel a pathogenic factor), rather than curing the illness, the pathogenic factor was instead pushed deeper into the body, creating a more severe illness in the future.
Note: Chinese medicine holds a similar perspective and argues that the defensive energy of the body which reacts to illness (the "Wei Qi)" functions to prevent external pathogenic factors from penetrating into the body. Chinese medicine in turn maps a progression of increasing severity of disease as the pathogenic factor travels from the superficial to the deep energy channels of the body (something I believe correlates with increasing blood stasis and loss of zeta potential obstructing larger and larger vessels). As such, Chinese Medicine's treatments are often aimed at expelling a pathogenic factor rather than counteracting the symptomatic reaction to it. Conversely, some schools of Chinese medicine advocated for suppressing the initial reaction to the more dangerous plagues (as this was lifesaving at the time), but acknowledged this resulted in a chronic infection in the future.
Throughout my career, I have seen numerous extremely compelling cases of Hering's Law of Cure (e.g., children with significant reactions to vaccines being given Tylenol for their fevers and then experiencing a much more severe illness, such as autistic regression, or COVID-19 patients crashing after their unpleasant fever is suppressed). Unfortunately, this principle remains largely unrecognized, and as a result, many standard medical practices are simply aggressive suppression of symptoms.
Note: Hering's Law of Cure subsequently expanded to recognize that the "deeper" layer of physical symptoms were emotional and mental in nature, and then even deeper ones were spiritual symptoms
The Global Loss of Vitality
Early on, when I began reading about the largely forgotten history of medicine, I was struck by two things:
• How profoundly damaging many of the early Allopathic remedies were (e.g., I've previously written about the smallpox vaccines, and this book does an excellent job at shedding light on the damage mercury did over the centuries).
• How much healthier people (who weren't poisoned by a mercury prescribing doctor) were and how much more effective many natural therapies were in the past than they are now.
This second point prompted me to begin asking older doctors (from various medical schools) if they had observed a general decline in human vitality in the patients they saw at the start of their careers compared to the end, and all of them shared that they had. Additionally:
• They noted that beyond patients becoming much sicker and having conditions they'd never seen before, it was also much harder to treat them as each therapy they used had shifted from making a dramatic improvement to a more minuscule one, which required numerous successive treatments to bring about an improvement.
• They typically attributed this shift to a loss in human vitality. They cited a variety of correlates (e.g., the average human body temperature dropping, people becoming less able to mount fevers, infants being less able to produce a brisk cry, or increasing degrees of fluid stagnation in their patients).
• They stated some of the treatments that had been developed by their profession were specifically made to address this loss of vitality, as their original treatments no longer worked. Conversely, some shared that when patients were placed in environments that restored aspects of their vitality (e.g., by being somewhere with exceptionally clean air), much less needed to be done to improve their condition.
•One doctor I spoke to had asked this same question of their mentor, while another had asked a mentor who'd also asked their mentor-all of whom corroborated that this decline in vitality had been continually in motion since at least the late 1800s.
Note: typically this decline in vitality proceeds in a linear fashion and then spikes at certain times (e.g., after the introduction of the smallpox vaccine, the 1986 law which granted immunity to vaccine manufacturers and led to a rapid proliferation in the vaccine schedule, and after the COVID vaccines). In each case, this increase in disease gets normalized and forgotten by the next generation of doctors (who entered practice after the last wave of sickness had become the "new normal") and by the time its noticed, it's often too late for them to share it (e.g., I was just speaking to a colleague who entered practice in the early 1970s and remarked that he used to have many patients in their 90s and 100s who were very mentally clear, that the dementia we frequently see in the elderly now was quite rare then, and that time it was rare to see cancers except in fairly old patients).
In turn, while I thought this model of decreasing vitality was valid (particularly since countless datasets have shown an explosion in the rates of chronic illness over the decades), it was much harder to say what was responsible as a good case could be made for so many different factors in our environment that the answer one arrived at was nearly guaranteed to be the product of one's biases and specific focus rather than an objective assessment. Nonetheless, when I asked a variety of skilled practitioners who'd successfully treated the "unsolvable" chronic illnesses over the decades, they shared that they typically found the root issue in those diseases was one of the following:
• Heavy metal toxicity
• Dental issues (particularly root canals).
• Pharmaceutical drugs
• Vaccines
• Chemical toxicity
• Dysfunctional dynamics perpetuating in their family constellation
• Electrosmog (e.g., EMF sensitivity)
• Toxic scars (e.g., from surgeries)
Note: while not a direct cause, many also believed the demineralization of our soil (which leads to nutritionally deficient foods) and modern technology making us be disconnected from all the natural rhythms that regulate the body were also major contributing factors.
When I looked at all of this, I realized a common thread over half shared was them creating fluid stagnation (or exacerbating the consequences of fluid stagnation such as insufficient nutrients being present in the remaining blood that reaches tissues-something, which for example, often underlies macular degeneration).
Next, since Chinese Medicine holds one of the longest medical records of humanity, I was curious to see if it had observed any significant changes in humanity's health and found out that around 1830, the concept of "blood stasis" became established as a primary cause of disease (and since that time has come to be seen as having a greater and greater importance). Since many of the highly unusual and severe injuries caused by the smallpox vaccine, introduced in 1796, matched those attributed to blood stasis in Chinese medicine, I looked up when it was first introduced to China-1805, which corroborates this theory.
Note: all of this could easily be expanded into multiple books. For those wishing to learn more, I covered the smallpox and blood stasis aspect of it in more detail here, the general loss of vitality here, how vaccines cause fluid stagnation here and the data demonstrating the profound damage vaccination has done to our society here.
Because of this, I am inclined to believe that the introduction of the smallpox vaccine (and the vaccines that followed) radically shifted humanity's health, and that much of this was a direct consequence of the fluid stagnation (e.g., due to a loss of physiologiczeta potential) that humanity experienced. However, while there is a good case for my argument, it could also be a product of my own biases, as my approach to medicine places a heavy emphasis on fluid stagnation, and I constantly see how it links to a myriad of diseases).
Systemic Suppression
Since it is often possible to make so many different credible and persuasive arguments for a topic at hand (e.g., what's causing this global loss of vitality), one of my approaches for filtering through them is seeing which ones then accurately predicted the future (as most don't ultimately pan out or are retroactively crafted to explain the past).
In turn, I've never forgotten a conference which happened in the 1970s (I believe it was in 1974) where one of the world's leading homeopaths convened a panel to discuss what the likely consequences would be in the upcoming decades of Allopathic medicine routinely suppressing symptoms (e.g., it aggressively treating all fevers with medications and preventing the childhood febrile illnesses with vaccination-something studies have repeatedly linked to cancer later in life).
Note: throughout the literature on the 1918 influenza, doctors from every school of medicine found influenza patients who had been treated with the fever suppressing medication aspirin (which was excessively distributed by MDs of the era) tended to be much more likely to die, while conversely, they discovered that the most effective treatments for the illness were those which then caused the fever to break on its own. Similarly, after I learned of the arguments against suppressing fevers, when I came down with a flu and did not feel well, I decided to try heating my body to see if it would accelerate the clearance of the infection and discovered not only that it did, but also that I immediately felt much better once I heated myself. This led me to conclude the discomfort the body experiences during a fever (assuming it is not an extreme fever) is not due to the heat, but rather the effort being expended to heat the body up and since then I've had many cases where heating the bodies (but not heads) of febrile patients greatly benefitted them.
At that conference, building upon Hering's Law of Cure (along with the recent mass introduction of suppressive steroids), they predicted that if Allopathic medicine continued to proliferate in its mass suppression of symptoms, in the decades to follow, we would see:
•We would see a global shift from less severe illnesses to more severe ones (e.g., cancers).
•That this suppression would cause physical illnesses to be pushed deeper into the body and be replaced with psychiatric illnesses, and in time spiritual ones (particularly when the psychiatric illnesses were also suppressed with medications).
Note: the predicted psychiatric illnesses included common ones (e.g., anxiety along with depression, which at the time was rarely an issue), psychopathy, mass shootings, self-harm and self-mutilation, and the public becoming willing to do crazier and crazier things. The spiritual ailments, included people wanting to be robotic rather than spiritually connected to life, and people knowing they were spiritually adrift because they'd lost their connection to life (which otherwise would have prevented much of this dysfunctional behavior).
It was hence quite noteworthy to me that many of these shifts indeed happened, and likewise to compare just how different patients in the 1970s (especially older ones) were. However, I also feel a very strong (albeit retrospective) case can be made that the increasing proliferation of vaccinations explains this shift.
All of the previous thus touches upon one of the central criticisms of Allopathic medicine: anytime an external agent is used to forcefully change a process which is unfolding within the body (rather than aiding the body's ability to resolve it) you run the risk of a minor temporary issue being exchanged for a severe chronic one-especially when this is repeatedly done throughout the course of someone's life. In some cases, this risk is very justified (e.g., in a life-threatening emergency or with a relatively safe drug that has limited long-term complications). At the same time however, a general unwillingness to acknowledge this issue pervades Allopathic medicine. Now everyone's gradually become habituated to patients "just being" sicker and sicker, and not much being possible to do about it.
Note: I believe this blindness arises in part because medical training requires doctors to be knowledgeable in a wide range of topics leading to many complex subjects being reduced to simple axiomatic truths that are memorized and then never questioned and because so much of the Allopathic therapeutic toolbox carries long term risks that it would be very difficult for doctors to practice medicine if they were fully conscious of those issues (discussed further here)
Suppressive Antibiotics
While steroids are one of the medications most associated with "suppressing" illness, many others are too. For example, for years, many natural medicine practitioners (e.g., homeopaths) also told me they'd frequently seen antibiotics "treat" an acute infection but turn it into a chronic one. I wasn't sure what to make of this (as microbiome disruption could partially but not fully explain it) then discovered something similar existed in Chinese Medicine::
The concept of Latent Heat is very old in Chinese medicine, having been mentioned for the first time in the 'Yellow Emperor's Classic of Internal Medicine'. Latent Heat occurs when an external pathogenic factor penetrates the body without causing apparent symptoms at the time; the pathogenic factor penetrates into the Interior, and 'incubates' there, turning into interior Heat. This Heat later emerges with acute symptoms of Heat: when it emerges, it is called Latent Heat.
Note: in modern Chinese Medicine, antibiotics and vaccines are now proposed as sources of latent heat.
Much later, when I read Cell Wall Deficient Forms all of this finally made sense. This book argued that when bacteria are exposed to lethal stressors, particularly cell wall destroying antibiotics, while most will die, some will instead enter a primitive survival mode and transform into misshapen cell wall deficient (CWD) "mycoplasma like" bacteria which can radically change their size or morphology (and hence look very different). While these bacteria are hard to detect (and when seen, due to no one knowing they "exist," often mistaken for cellular debris and ignored), with the correct techniques they can be detected. In turn, the book provides a wealth of evidence that CWD bacteria:
• Are found within many "aseptic" tissues undergoing an autoimmune attack, with specific CWD bacteria associated with many different autoimmune disorders which have no known cause.
• Once the environment is "safe" can transform back into their normal form and cause a sudden recurrence of an infection-suggesting chronic infections are due to antibiotics creating a dormant CWD population rather than continual reinfection.
Note: many popular alternative schools of medicine (e.g., those of Rife, Naessens, and Enderlein) came from microscopes which could directly observe these pleomorphic bacteria continually shifting into new morphologies, and that diseases states (e.g., cancer) correlated to specific morphologies, while other morphologies resulted in a symbiotic state of health (e.g., this a video of the organisms Naessens observed). Since the morphologies adopted correlated with the internal state of the body, this gave rise to the belief that treatments should aim to create "healthy terrains" within the body, which would give rise to non-pathogenic forms of the bacteria rather than antibiotics that provoked pathogen transformation.
All of this has influenced how I (and quite a few colleagues) practice medicine in some unique ways:
• First, around 10% of chronic conditions I come across seem to have a "pleomorphic" component and improve once that is addressed.
• Second, while sometimes helpful and necessary, I try to avoid using cell wall targeting antibiotics (e.g., penicillin) as they are particularly prone to provoking the CWD transformation.
• Third, I have found many therapies which help autoimmune conditions (e.g., ultraviolet blood irradiation) often also happen to be highly lethal to CWD. As such. I have long wondered if certain rheumatologic drugs work in this manner. For example, there was a prolonged period where minocycline (which is potent against mycoplasma) was successfully used to treat rheumatoid arthritis (RA), but eventually abandoned as (like all tetracycles) it had some side effects, it only worked in a subset of RA cases but not others, and there was no mechanism to explain how it could be working.
Note: a case has been made that there are widespread mycoplasmal infections in the population (that possibly were lab engineered). The drug that best treated those infections was doxycycline, and I have long wondered if the reason why integrative practitioners find it helps inflammatory conditions like Lyme disease is because it is actually eliminating pathogenic mycoplasma.
Likewise, one of the most popular drugs in rheumatology, methotrexate, "works" by depleting folate production in the body, but oddly still works when folate is given to counter (some but not all) of its side effects-implying folate elimination is not its actual mechanism. Conversely however, it also has potent antibacterial properties ( against specific bacteria), and rather than targeting the cell wall, it reduces bacterial DNA synthesis.
Note: many integrative physicians find that chronic autoimmune illnesses are linked to a wide range of chronic but unrecognized infections (possibly because the organisms contain antigen sequences matching normal tissue and hence provoking an autoimmune attack against it).
Cortisol
To regulate itself, the body often relies upon sensors that detect something amiss and then emit a signal that is amplified by the body so that a process can be set in motion to fix the issue that set the sensor off. One of the key signals the body relies upon are hormones, as small amounts of these molecules being released are often sufficient to change the internal state of the body drastically.
The hypothalamic-pituitary-adrenal (HPA) axis is the body's central stress response system. It involves three main components: the hypothalamus and pituitary gland in the brain, and the adrenal glands on top of the kidneys. When you experience stress, the hypothalamus releases corticotropin-releasing hormone (CRH), which signals the pituitary gland to secrete adrenocorticotropic hormone (ACTH). ACTH then travels through the bloodstream to the adrenal glands, prompting them to release the corticosteroid cortisol (the body's primary stress hormone). Finally, once cortisol levels are high enough, they signal the brain to reduce CRH and ACTH production, creating a negative feedback loop that prevents over-activation of the stress response.
Cortisol, in turn, has a few key functions in the body:
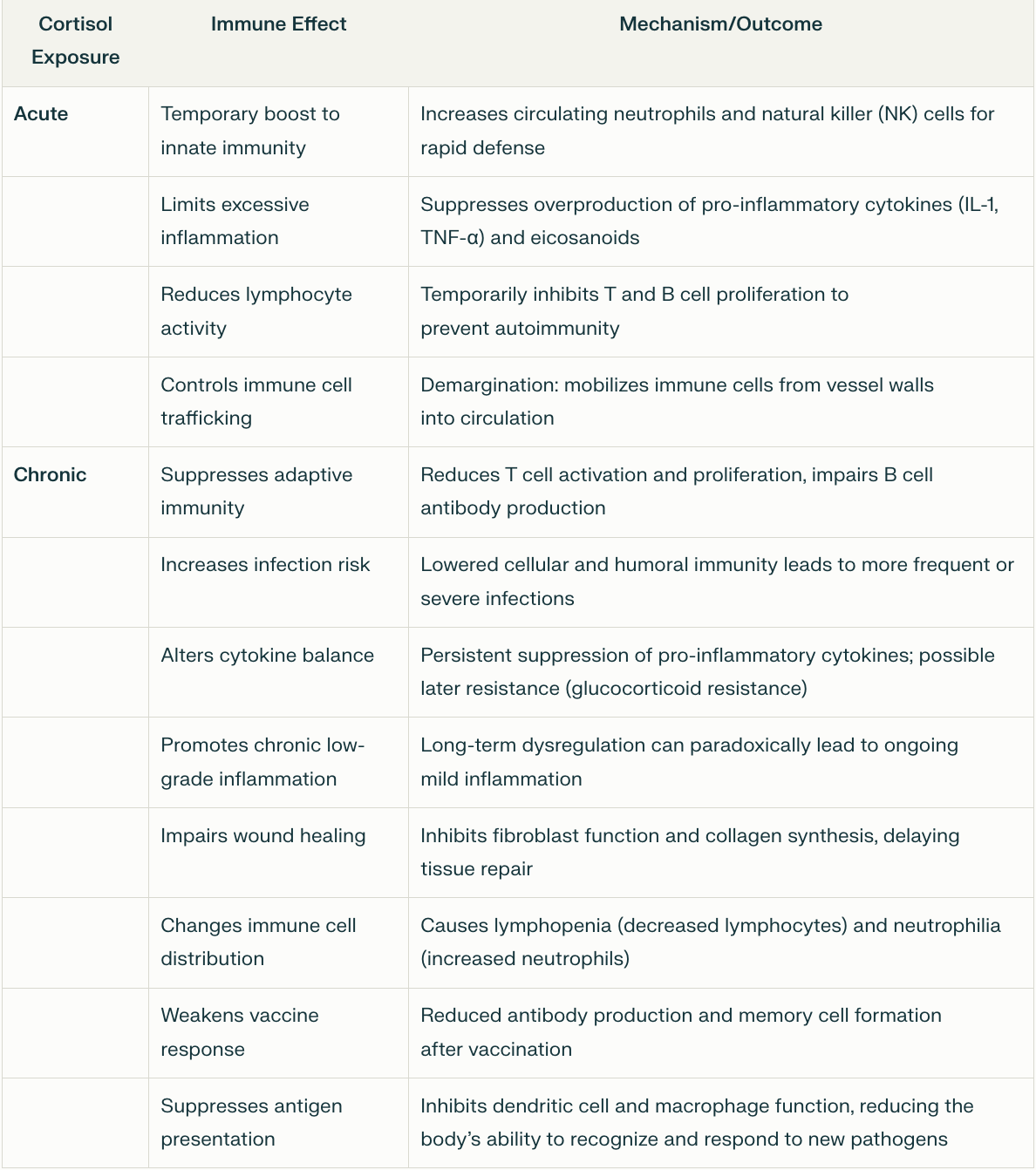
Immune Modulation: Cortisol enhances the immune system's immediate response to threats (protecting the body during stress) while limiting excessive immune activity to prevent autoimmunity. It does this partly by inhibiting pro-inflammatory cytokines (e.g., IL-1, IL-6) and reducing T-cell activity. Over time, this shifts to immune suppression, making synthetic corticosteroids, a popular treatment for inflammation and autoimmunity.
Note: at lower doses, this transition from immune stimulation to immune suppression takes much longer, whereas at high doses it's faster (hence why high steroid doses are given for autoimmune flares).
Blood Sugar: When blood sugar is low, cortisol raises it by stimulating gluconeogenesis in the liver, mobilizing amino acids (from muscle) and fatty acids (from fat) for glucose production, and reducing insulin sensitivity in tissues like muscle and fat. Excessive cortisol can lead to diabetes, abdominal fat accumulation (obesity), weight gain, insulin resistance, and cardiovascular issues.
Connective Tissues: Cortisol promotes protein catabolism (breakdown) in muscles to provide substrates for glucose synthesis and inhibits collagen synthesis. Excessive cortisol causes muscle wasting, bone loss (e.g., osteoporosis or osteonecrosis), poor wound healing (which is also a result of immune suppression), skin thinning, easy bruising, and purple striae.
Circulation: Cortisol raises blood pressure by increasing sodium and water retention, sensitizing blood vessels to epinephrine and norepinephrine, which causes vasoconstriction and an increased heart rate, while also damaging the blood vessel lining. This elevates the risk for cardiovascular disease 1, 2, 3 (e.g., a one standard deviation increase in morning plasma cortisol is linked to an 18% higher risk of future cardiovascular events).
Cognition: Cortisol modulates arousal, attention, and memory consolidation. Chronic excess corticosteroids (from either endogenous cortisol or synthetic steroids) impair hippocampal function, causing memory deficits, increased pain sensitivity, attention issues, cravings for high-calorie foods, substance abuse, and, rarely, psychosis.
HPA Axis Dysfunction: Since the HPA axis is regulated by cortisol levels, once they are chronically elevated, the HPA axis becomes desensitized to cortisol (leading to excessive cortisol secretion) or loses the ability to secrete cortisol when needed. This in turn creates many issues such as the previously described ones associated with chronically excessively cortisol levels and varying degrees of fatigue (e.g., due to the adrenal glands not secreting cortisol when needed). Additionally, this dysregulation can often last for months once the excessive cortisol levels drop.
Note: excessive cortisol can also cause other effects such as blood electrolyte imbalances, alkalosis, cataracts, and glaucoma.
Because of this, many believe excessive cortisol secretion and HPA axis dysfunction (e.g., due to chronic stress, poor diet, poor sleep, alcoholism, too many stimulants like caffeine, social isolation, a lack of exercise, or irregular daily rhythms) is the root cause of disease. As such, they advocate for lifestyle practices that counteract these HPA axis-disrupting factors, and in many cases significant health benefits follow the adoption of those practices.
Note: a variety of medical conditions (such as a tumor that continually secretes the hormone that triggers cortisol production) can cause excessive cortisol levels. Many of the symptoms described in this section were discovered from studying those conditions.
Corticosteroids
The hormone cortisol belongs to a class of steroids known as corticosteroids, due to their release by the cortex of the adrenal glands. While many related corticosteroids (henceforth referred to as "steroids") exist within the body, the body's primary ones are cortisol (a glucocorticoid) and aldosterone, a mineralocorticoid which regulates blood pressure, volume, and electrolyte balance.
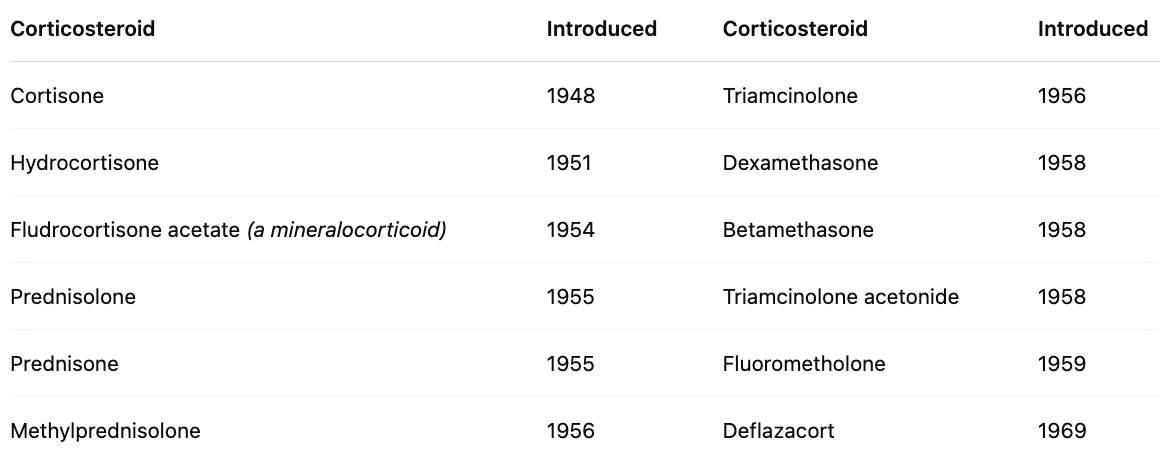
In 1946, the first synthetic steroid (cortisone) was synthesized. Two years later, enough had been produced to test on it a human, where it was discovered to improve rheumatoid arthritis symptoms (which won the 1950 Nobel Prize) and was immediately hailed as a 'wonder drug.' Before long, it was discovered that other inflammatory syndromes also responded to cortisone, and a rush of other steroids hit the market:
Following its success in rheumatoid arthritis, steroids (e.g., prednisone, hydrocortisone) were rapidly adopted for a wide range of inflammatory and autoimmune disorders, including systemic lupus erythematosus, inflammatory bowel disease, and multiple sclerosis, due to their ability to suppress immune-mediated tissue damage.
According to the sources I looked at, in the early 1950s, steroids were hailed as a revolutionary treatment for those conditions (and hence widely prescribed), with new steroids (e.g., prednisone) being rapidly introduced to the market, but in the late 1950s, serious side effects began to accumulate from long-term steroid use. By the early 1960s, steroid treatment was ' 'shunned altogether by the rheumatology community" (to the point shortly after that NSAIDs like ibuprofen were named non-steroidal anti-inflammatory drugs to distinguish them from the disastrous steroids) after which point steroids were prescribed with more caution and at lower doses until it was reborn in the 1980s under a low dose regimen.
Note: I am not completely sure about this timeline, as I know steroids were widely used in the 1970s (at least in certain parts of the country) and patients were rarely informed of their dangers. Likewise, I still frequently encounter doctors who are unaware of the dangers of these drugs and will "throw prednisone" at any unusual symptomatology a patient is suffering from that appears to be immunological in nature (which in some cases that I've never forgotten, was disastrous and caused permanent complications for the patient).
Currently, steroids remain widely used, and their use has gradually increased. For example, in 2009, 6.4% of American adults had used oral steroids at least once in the last year, whereas in 2018, 7.7% did, while a 2017 study found 21.4% of adults (age 18-64) had used at least one oral steroid prescription in the last three years.
Note: after harms were discovered with steroids, the pivot made to protect them was that they are safe if "low doses" are given. However, over the decades, what constituted a safe "low dose" has greatly declined (i.e., doses now considered toxic previously were routinely prescribed), and that drop will likely continue to (e.g., in 2016, Europe's Rheumatology group concluded in was unsafe to give more than 5mg a day of long-term steroids—a figure significantly lower than the current amount used in America).
Steroid Side Effects
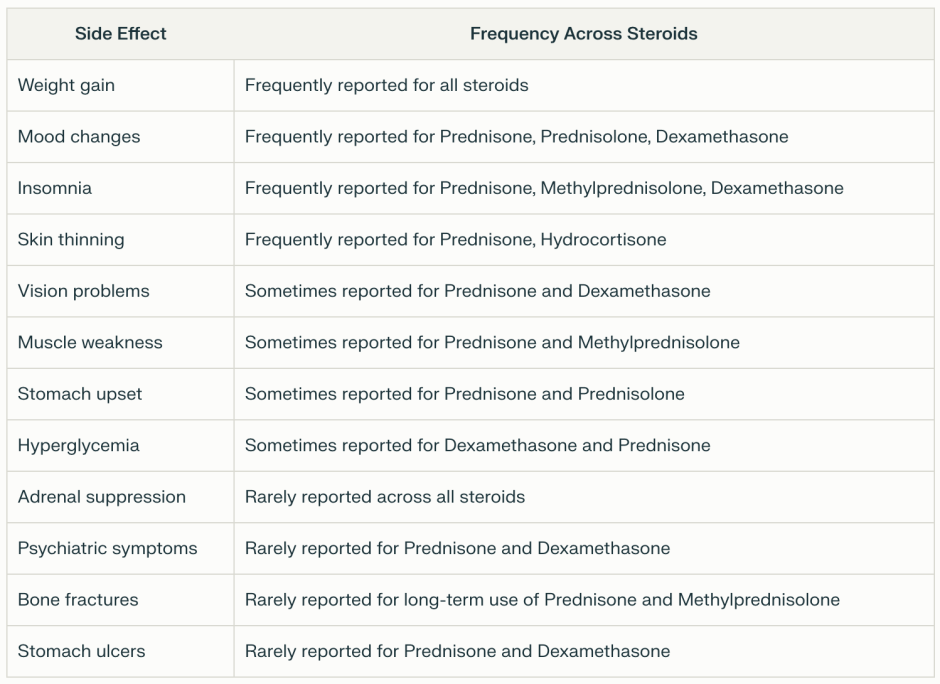
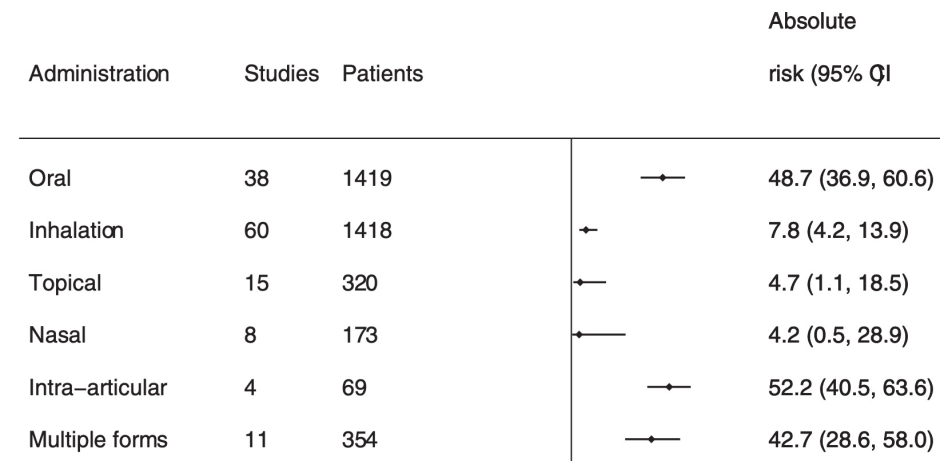
Steroids can be administered through a variety of routes (e.g., topically, orally, inhaled, injected, or intravenously). Generally speaking, shorter and more external courses of steroids are less likely to cause problems, while longer ones (particularly oral routes) tend to cause the most issues. As you would expect, the side effects from taking steroids mirror those seen with excessive cortisol, although in many cases they are much more severe.
Furthermore, they are quite common (e.g., one study found 90% of users report adverse effects, and 55% report at least one that is very bothersome). Likewise, this (AI-generated) summary of what users across the internet have reported mirrors what we've seen over the years:
- Weight Gain and Increased Appetite: Almost universally reported, often one of the first side effects noticed. Users frequently discuss rapid weight gain and intense hunger, especially early in treatment or with higher doses.
- Mood Changes and Mental Health Issues: Extremely common, with mood swings, irritability, anxiety, and depression mentioned in many posts. Severe effects like suicidal thoughts are less frequent but still notable, particularly at high doses.
- Insomnia and Sleep Disturbances: Very frequently reported, often tied to evening doses. Users regularly describe trouble falling asleep, vivid dreams, or waking up repeatedly.
- Fatigue and Weakness: A common complaint, especially during long-term use or tapering. Many report feeling drained despite the drug's anti-inflammatory effects, often linked to adrenal issues. Dizziness is also reported.
- Skin and Hair Changes: Thin skin, bruising, acne, and stretch marks are often discussed, as are hair thinning or excess body hair, particularly among women on longer courses.
- Digestive Problems: Indigestion, stomach pain, and nausea are regularly mentioned, especially when doses are taken without food. Ulcers or reflux are less common but still noted.
- Bone and Joint Issues: Joint pain and muscle aches are fairly common, with osteoporosis or fractures discussed more by long-term users, reflecting concerns about cumulative damage.
- Cushingoid Features: Moon face, buffalo hump, and abdominal fat are frequently mentioned by those on prolonged therapy, often tied to emotional distress over appearance changes.
- Increased Infection Risk: Recurrent infections like colds or UTIs are commonly reported, though less dominant than weight or mood issues, and more prominent with higher doses.
- Blood Sugar and Diabetes: Elevated blood sugar is noted, especially by those with diabetes or on long-term treatment, but it's less universally discussed than physical or emotional effects.
- Withdrawal Symptoms: Fatigue, joint pain, and nausea during tapering are often shared, but these are more specific to users reducing doses after extended use, so less broadly reported.
- Vision Problems: Blurred vision, cataracts, or glaucoma are mentioned occasionally, typically by long-term or high-dose users, making them among the least frequently reported.
Note: I used to spend months reading through online support groups for pharmaceutical injuries, and thus find it incredible AI tools can rapidly summarize all of those postings.
Likewise, many of those effects have been established within the scientific literature:
Bone Loss: Corticosteroids double one's risk of a fracture (and even more so for a vertebra), with 12% of users reporting fractures. At typical doses, steroids cause a 5-15% loss of bone each year, and in long-term users, 37% experience vertebral fractures (additionally, high dose steroid use increases the risk of vertebral fractures fivefold). Steroid bone loss in fact, is such a common problem that treating it is one of the few official indications the FDA provides for bisphosphonates (which while widely prescribed for bone loss have many severe side effects—including making your bones more likely to break). Lastly, higher doses increase the likelihood of avascular necrosis (with 6.7% of users taking higher steroid doses developing it).
Note: we saw one patient who developed avascular necrosis (bone death) in both hips following a course of steroids and most likely would have in both shoulders had treatment not been initiated.
Weight Gain: a pproximately 70% of individuals taking oral corticosteroids long-term (over 60 days) report weight gain. One study found a 5.73-12.79 lb increase per year, and another found a 4-8% increase in body weight after two years of steroid use. Additionally, this fat typically stores in areas like the face, neck, and belly.
Adrenal Insufficiency: corticosteroids reduce the adrenal gland's ability to produce cortisol (which can sometimes be life threatening), and increases with the duration of therapy and their route of administration (e.g., affecting 48.7% of oral users).
Diabetes: a systematic review found individuals taking systemic corticosteroids were 2.6 times more likely to develop hyperglycemia (with 1.8% of those receiving steroids in a hospital then developing diabetes). Likewise, another study found that patients who'd taken systemic corticosteroids at least once were 1.85 times more likely to develop diabetes. Finally, a meta-analysis found that, in patients without pre-existing diabetes, a month or more of steroids caused hyperglycaemia in 32% and diabetes mellitus in 19% of them.
Cardiovascular: high doses of steroids have been observed to increase heart attacks by 226%, heart failure by 272%, and strokes by 73%.
Eyes: Steroids have been found to increase the risk of cataracts by 245-311% (with 15% of users reporting this side effect) and the risk of ocular hypertension or open angle glaucoma by 41%.
Gastrointestinal: Steroids are linked to many gastrointestinal events (e.g., nausea and vomiting) and have been found to increase the risk of gastrointestinal bleeding or perforation by 40%.
Psychiatric: between 1.3%-18.4% of steroid users develop psychiatric reactions (with the rates increasing with the dose), and around 5.7% experience severe reactions. Mania and hypomania are the most common reactions, while the risk of depression increases with prolonged usage. Additionally, 61% of steroid users reported sleep disturbances, and steroids can also sometimes cause psychosis. 1, 2
Infections: Steroids also increase the risk of infections. For example, users of inhaled steroids were found to be 20% more likely to develop tuberculosis, and this increased at higher doses in patients with asthma or COPD. Similarly, patients on steroids were 20% more likely to develop sepsis (possibly due to the initial symptoms of the infection being masked by the steroids).
Skin: prolonged topical use of steroids also frequently causes skin issues (e.g., up to 5% experience skin atrophy after a year of use).
Note: in the mid-1960s, while steroids were still being widely promoted by the medical field, one of my colleagues did an oral steroid study on mice and saw they had breakdown of collagen along with fatty or degenerative of the major organs (e.g., liver and heart) which caused them to change their career path.
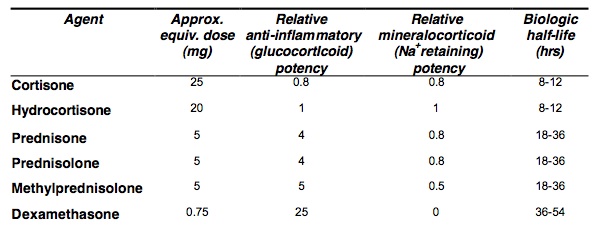
Lastly, it's helpful to know that certain steroids are much more potent than others and that the more potent ones that persist in the body (e.g., dexamethasone) are more likely to create systemic effects like HPA axis dysfunction.
Uses for Steroids
In short, all of this argues that steroids, if used, should only be done when necessary, be given at the lowest dose, and the patients carefully monitored for side effects (much of which does not occur in practice). Let's now look at how they are currently being used.
Inhaled Steroids
Inhaled steroids are routinely used to treat asthma and COPD. Since the systemic absorption of inhaled steroids is much less than from oral steroids, systemic side effects are rarer (but can still occur with prolonged use at higher doses). Instead most of the side effects are concentrated in the airway (e.g., oral thrush from candida, a sore mouth or throat, a hoarse or croaky voice, cough, dry mouth or throat, throat irritation, pain, or need for throat clearing, altered sense of taste or bitter taste, thirst).
While inhaled steroids (along with the other medications commonly prescribed for these conditions) can help and are often the only option available to patients, I believe in most cases natural therapies which directly treat the conditions are preferable. For example, COPD is seen as a progressive and incurable illness which can only be delayed or partially mitigated with the existing therapies. In contrast, when nebulized glutathione is used to replenish the protective lining of the lungs (explained further here), it halts the progression of the disease, and unlike steroids does so without side effects. Likewise, many natural therapies exist for asthma.
Topical Steroids
Topical steroids are routinely used for skin issues and sometimes in other areas as well, such as for certain eye conditions, like preventing graft rejection after a necessary corneal transplant. In these instances, systemic side effects are rare, and most of the local issues result from prolonged use (e.g., skin changes or skin thinning—particularly on the face). While I can't prove this, I have long suspected topical steroids in part work by reducing fluid circulation to the skin ( via the insterstitium), thereby preventing inflammatory toxins from arriving there and creating skin reactions (whereas agents like DMSO treat skin conditions by augmenting the circulation within the interstitium so stagnant toxins cannot irritate a set area).
Note: for the reasons outlined earlier in this article (e.g., Hering's Law of Cure), I tend to avoid treating skin issues with topical steroids (particularly since there is often an underlying cause of skin eruptions that can be discerned and addressed). However, to the best of my knowledge, this has not been studied (and given the way research topics are chosen, is unlikely to be in the future).
Injectable Steroids
Frequently, when patients have significant pain in a joint, steroids will be injected into the joint to improve the pain. I believe there are three significant issues with this approach.
First, a certain degree of systemic absorption occurs, so many of the previously mentioned side effects can follow steroid injections (e.g., high blood sugar for over a week).
Second, if the injected steroid is not water soluble (most aren't), it will often remain in the joint (e.g., you can often see previously injected steroids within a joint when it is arthroscopically) examined.
Third, steroids weaken and degrade connective tissue (e.g., the ligaments holding a joint together). Since arthritis often results from weakened ligaments no longer holding the joint in the correct position (causing it to grind against itself when it moves), this creates a situation where a temporary relief is gained from the steroid that is followed by a worsening of the underlying issues, which then typically results in the patient eventually needing surgery. This is particularly problematic in the spine as the spinal surgeries which follow frequently leave patients much worse off (and can often be avoided if the spine is strengthened rather than weakened—all of which is discussed further here).
Note: in some cases, I've found the benefit patients receive from joint injections results from the local anesthetic (e.g., lidocaine) mixed with the steroid (due to its temporary anesthesia resetting a hypersensitive nerve), which makes it even more unfortunate that an unnecessary and harmful steroid was injected.
Lastly, it is important to note that many (and arguably the majority) of joint issues have an inflammatory component (e.g., many patients have undiagnosed seronegative spondyloarthropathies that often do not show up on standard diagnostic tests). On the one hand, this illustrates why both conventional and natural approaches for reducing inflammation can help with so many different joint issues. Conversely, it also helps explain why joint issues increase with age, as inflammation and metabolic healthworsen with age.
Intravenous Steroids
Certain more severe illnesses respond to steroids, and as a result intravenous steroids are routinely given to certain hospitalized patients. In those instances (especially given the options available for hospitalized patients), this is often necessary and lifesaving. At the same time however, as shown above, this approach can have significant side effects.
Oral Steroids
Oral steroids have the widest range of diseases they are used to treat, which is unfortunate since they also tend to cause the most side effects. Some of their common uses include:
•Severe cases of chronic lung conditions (e.g., asthma or COPD).
•Allergic reactions of varying severity.
•Various rheumatologic disorders, along with many other autoimmune conditions such as inflammatory bowel diseases and certain blood disorders.
•Preventing the rejection of transplanted organs.
•Replacing hormones that the adrenal glands have lost the ability to produce.
•Certain skin disorders.
•For disc herniations, along with other acute musculoskeletal issues like gout, bursitis, or tendonitis that are not responding to NSAIDs, or to reduce swelling and pain from a recent severe injury.
While some of these are justified, a strong case can be made that many others cause more harm than any benefit they provide.
Using Steroids In Practice
Over the years, I've found a wide range of perspectives on the use of steroids in medicine, ranging from a great reluctance to prescribe them to a general support for them. For that reason, I felt it was important to share the perspective of a few different specialists I respect, who have used a lot of steroids during their career and since COVID drifted towards integrative therapies.
The first comes from a rheumatologist:
Early in my career I used a lot of steroids but I now almost entirely avoid them because they have too much toxicity from long-term use. While there is increasing awareness of the dangers of these drugs, I feel my speciality still do not fully appreciate how dangerous they are or that many conventional and holistic alternatives now exist to steroids that get the same results without most of their side effects. Worse still, steroids are far too popular with primary care providers due to the immediate benefits they create and a lack of awareness about the long term consequences they create.At this point, the main situation I would use steroids in is if I have a patient with a life-threatening autoimmune exacerbation (e.g., lupus shutting down the kidneys, lupus cerebritis affecting the brain or a systemic vasculitis), and the steroids would be done briefly to stabilize them and serve as a bridge before you switch to something less toxic. I feel a case can also be made for using them for classic Rheumatologic emergencies that require steroids like temporal arteritis putting a patient at risk of blindness (especially if any vision loss has already occurred), but in those cases, there is often another drug that can treat it as well.
Note: this rheumatologist also believes NSAIDs (which many rheumatologists routinely use) are greatly over prescribed and due to the deaths they cause, should not be available over the counter (as this leads to excessive doses of them frequently being used) and should only be used sparingly as needed (rather than being prescribed on a set daily dose). For those interested, the dangers of NSAIDS are discussed further here.
The second comes from an orthopedic surgeon:
In my experience, giving steroids accelerates the degeneration of a joint, so whenever a patient requests an injection, I warn them about the deal they are making and that it's likely a joint replacement will follow. I try to avoid unnecessary surgeries, so I am "incentivized" to give this advice, whereas I find many orthopedists act differently as their salary depends upon frequent surgeries. Typically the main reason I'll use injectable steroids is if the patient really needs a temporary improvement in the joint and I feel it's unlikely it will be possible to address the root causes of their condition.
The third comes from a surgeon who also worked as an ICU doctor:
I've used systemic steroids for adrenal insufficiency in patients dying of circulatory collapse (refractory shock) after massive sepsis or injury and it can be amazing for over 20 years. However the subsequent infectious complications that often occur temper the long term success for these patients- i.e., they often live through the crisis, but then often are lost or severely debilitated from infectious complications that result from the high dose steroids needed. I no longer work in an ICU setting, but I have recently learned of an older product (methylene blue) which has been used for refractory shock and does not have the same infectious complications.Prolonged use of systemic steroids significantly increases solid cancer risks and as a practicing surgeon it was impossible to not notice the worse outcomes these same patients had with their increased cancer for basically every metric (cure rate, recurrence rate, wound infection rate, response to therapy, etc...).
The fourth comes from a dermatologist:
Generally speaking, topical steroids are very safe, and I believe many of the concerns with them arose from the fact alternative treatment options did not exist in the 1970s, so steroids were overused and data hence accumulated at that time showing their adverse effects, particularly since more potent ones were frequently used (especially on the face, armpit or groin which we know are more sensitive to steroids). I do see the consequences of topical steroid overuse (e.g., skin thinning and hypopigmentation) but it's rare.I try to avoid oral steroids entirely as they have real risks (e.g., I've seen too many patients who developed Cushing's or Cushing's like syndromes from oral steroids given for a lung condition) and better alternatives exist for those diseases now. The last time I prescribed oral steroids was a few months ago for a fairly rare skin disease where it was indicated, and I believe that they are very helpful allergic contact dermatitis (e.g., poison ivy) but those patients are normally treated long before they see a dermatologist.
With oral steroids, the primary issue I encounter are patients (typically at the emergency department) being prescribed a brief course of oral steroids for an undiagnosed rash, and then after it gives them brief relief seeing another ED doctor who does the same thing, often at a different dose (since there is little standardization in steroid dosing). Additionally, certain diseases (e.g., psoriasis) that sometimes receive oral steroids should not be treated with oral steroids (as it becomes worse once the steroid is stopped), but these cases tend to be rarer (e.g., most psoriasis patients eventually get diagnosed and there are much better treatments for the condition than steroids now).
With topical steroids, the most common problem is that they're reflexively given for skin issues (e.g., by primary care providers), and in some cases the skin issue is incorrectly diagnosed and the topical steroids are given where they are inappropriate, often providing brief relief but ultimately make things worse (e.g., if an "autoimmune" rash is actually fungal in nature). Unfortunately, many doctors (particularly ER ones who rarely have access to a dermatologist they can consult) will prescribe steroids despite not being sure of the diagnosis. Lastly, there are some tricks to appropriately dosing topical steroids for skin conditions that are not well understood by general practitioners.
The fifth comes from an integrative physician with a focus on gastroenterology:
Steroids are the ultimate bandaid which will put out a fire, but then will deteriorate your immune system, heart, liver, kidneys and bone (and in one case I never forgot, I saw a highly muscular man who was on the highest steroid dose I've ever seen—100mg/day—gradually have all his muscles wasted away).Some people think a short low-done course of steroids is worth doing but I don't because some people will react to it and in most instances, I only use steroids because patients I see are on them, and in those cases I try to taper them off. The only oral steroid I ever use is betamethasone because it has poor gastrointestinal absorption and hence can sometimes be used for gut inflammation without significant systemic side effects.
The sixth comes from a psychiatrist:
Steroids can trigger mania and hypomania, but unlike in bipolar, this normally comes on gradually. When it comes on gradually, at the start, like other types of substance induced mania, the patient can often realize something is "off" and may seek help. In hospital settings (where high steroid doses are often used) psychiatric changes tends to come on much faster and are often missed. Since hospitals (especially now that declining funding has made them be tightly packed and full of disorienting alarms and light all throughout the day) are an environment which is conducive to delirium, we often see steroids induced psychiatric changes then evolve into psychosis and delirium.As delirium responds best if treated early and greatly worsens patient outcomes, I have long believed if every patient receiving high dose steroids was screened for the initial hypomania, it would greatly improve patient morbidity and mortality.
To address all of this, there are three main strategies I use. First, assess if the steroids are necessary (e.g., a life threatening autoimmune condition), and if not stop them. Second, in many cases, especially outside of a hospital, if you fix the patient's sleep (ie. with a short course of a sleeping aid), that is sufficient to resolve the personality changes. Finally, if medication is needed to treat it (e.g., in the hospital), Zyprexa is the most consistently effective option.
Additionally, in patients with schizophrenia, steroids can often worsen an existing psychosis. Steroids also tend to increase blood sugar levels, and since many of the medications for schizophrenia (e.g., Zyprexa) can cause metabolic syndromes (e.g., diabetes), when these patients are hospitalized and given steroids, it is often necessary to use higher insulin levels than they take at home (and hence continually adjust their insulin dosing to their current blood sugars).
Overall, I feel steroids can be helpful in certain situations (e.g., I refused to use a steroid after a bursitis triggered by prolonged overexertion, and because of that it never fully healed after that temporary overexertion, and frequently they are needed for life threatening autoimmune flares), but at the same time, I typically avoid them.
The seventh comes from an ER doctor:
In the right clinical context, steroids can be life-saving-especially for acute respiratory conditions like severe asthma, COPD exacerbations, or for patients in septic shock. In the emergency room, we routinely administer steroids for these situations. Occasionally, I also encounter less common scenarios where steroids are necessary, such as when a brain tumor causes compression and swelling; in these cases, steroids help reduce intracranial pressure.However, there are also situations in the ER where the decision to use steroids is less straightforward, and it's not always clear whether the potential benefits outweigh the risks.
I strongly support the acute, short-term use of steroids. But when they are used for more than 5-7 days, significant problems can arise-such as chronic tissue weakening and adrenal suppression. In my opinion, one of the biggest misconceptions in orthopedic medicine is encouraging patients to "try" one to three steroid injections for knee pain, as these patients often end up needing a knee replacement within a year anyway. A similar issue exists with steroid injections for spinal pain, where the long-term surgical consequences can be even more severe.
It's also important to recognize that different steroids have varying degrees of mineralocorticoid (blood pressure-raising) and glucocorticoid (anti-inflammatory) activity. Choosing the right steroid for the specific clinical situation is crucial to optimizing patient outcomes.
The final comes from a pulmonologist and ICU doctor:
Throughout my career, I've given steroids to thousands of patients and except for one case where they developed myopathy, all of the side effects (e.g., feeling bad) were self-limited and stopped once the steroid was stopped. In my specialty, we regularly use steroids and see their benefits, but I feel there is too much fear around systemic steroids, so many specialties (besides rheumatology) often won't touch them and as a result, many patients don't receive the immense benefits they could receive from them. In my experience systemic steroids are most useful with:•Any hospital-level infection (e.g., sepsis) provided they are on the appropriate antimicrobial therapy.
•COPD and asthma exacerbations.
•Certain anaphylaxis cases.
•Inflammatory brain disease (e.g., two of my family members with PANDAS got their lives back after a course of oral steroids).
•Patients with severe asthma or COPD which does not respond to other treatments (which is rare, but in those cases low dose prednisone got them their lives back).
Lastly, my experience thus far has been that steroids rarely help vaccine injured patients.
All of these perspectives in turn touch upon two important truths. First, nothing is black and white in medicine, and an argument can hence be made for or against steroids. Secondly, I believe it is almost impossible to avoid the trap of perceptual biases (particularly those which argue against a drug one routinely prescribes), as these doctors saw significantly different adverse outcomes from large pools of patients (and likewise other colleagues who largely avoid steroids have noticed even worse effects from steroids during their career).
In my eyes, the central issue with steroids is that while they do suppress the immune system (which is sometimes needed), they are too broad in their effects, and as a result, in most conditions, a significant number of unwanted consequences inevitably happen from their use.
Alternatives to Steroids
Something often difficult to appreciate about medicine is just how much remains to be discovered, and how frequently something which seems revolutionary at the time later becomes clearly wrong or is replaced with a radically superior alternative.
For example, many do not know that Anthony Fauci is immensely respected throughout the rheumatologic field because shortly after he joined the NIH in 1968, he had the insight that chemotherapy drugs (which destroyed the white blood cells at standard doses), when given at low doses could instead be used to suppress dangerous autoimmune responses. This worked, and cyclophosphamide allowed certain previously incurable diseases to become very manageable (e.g., 90-98% of patients who had granulomatosis with polyangiitis died within 1-2 years of diagnosis, while with the low dose chemotherapy the remission rate went from 0 to 93%).
Many of those drugs were not at all safe (e.g., cyclophosphamide often gives you cancer), but compared to the previously existing options were revolutionary, and as such, immune suppressing drugs which created various consequences of immune suppression (e.g., cancer or frequent and unusual infections) were seen as completely justified and hence became the standard of care.
Note: the drug Fauci pioneered for life threatening vasculitides, cyclophosphamide, is still used in that manner (as it is lifesaving) but never received an FDA approval for it (which is noteworthy given how aggressively Fauci targeted "unapproved" therapies during the AIDS crisis and COVID-19).
Fortunately, since that time, the success of the steroids and chemotherapy drugs in suppressing dangerous immunological processes helped pave the way for drugs which could selectively target aspects of the immune system rather than everything, thereby allowing potent agents to be developed with significantly less side effects (although many of the drugs routinely used to treat autoimmune conditions still have significant side effects).
In tandem with this, a variety of more natural approaches have been developed over the years that often effectively treat a wide range of autoimmune disorders that were not available in the past (along with many of the other things steroids treat such as musculoskeletal issues).
Because of this, I feel it's fairly rare that systemic steroids are necessary, and in most of the instances where they are (outside of life-threatening circumstances), low and short doses with fewer side effects should be used.